
Healthcare / Home Health
& Long-Term Care

Regional Managed Care Provider and Care Coordination Network supporting 100K+ patient visits monthly

Invoice Review, Reimbursement
Validation, and Compliance
Monitoring
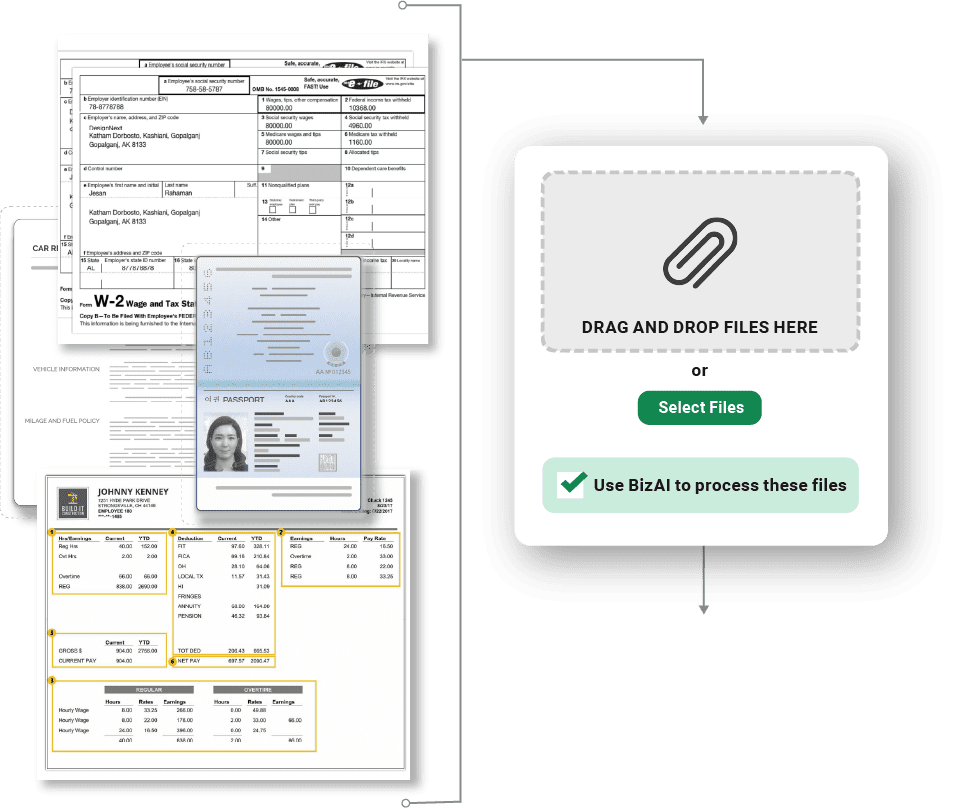
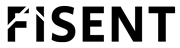
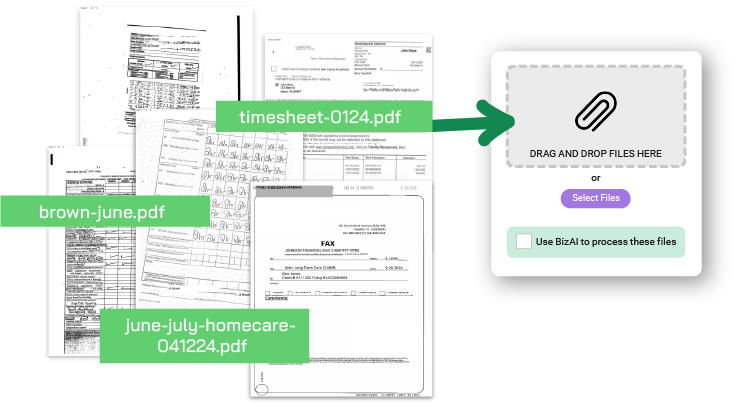
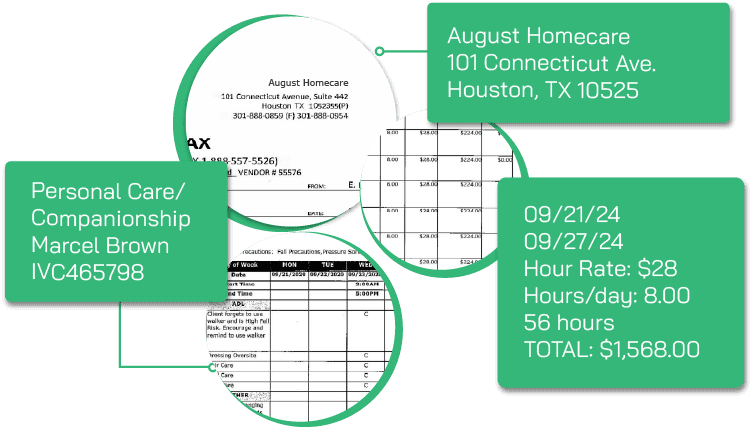
Caregiver invoices submitted for reimbursement include a wide range of services, care codes, and supporting documentation. These invoices are often unstructured — arriving via email, portals, or fax — and contain complex details that must be verified against contract terms, approved care plans, and payer policies.
Operations and compliance teams faced several persistent challenges:
The result: longer reimbursement cycles, increased operational risk, and inconsistent service provider experience.
Fisent BizAI automates the ingestion, review, and processing of all caregiver invoices.
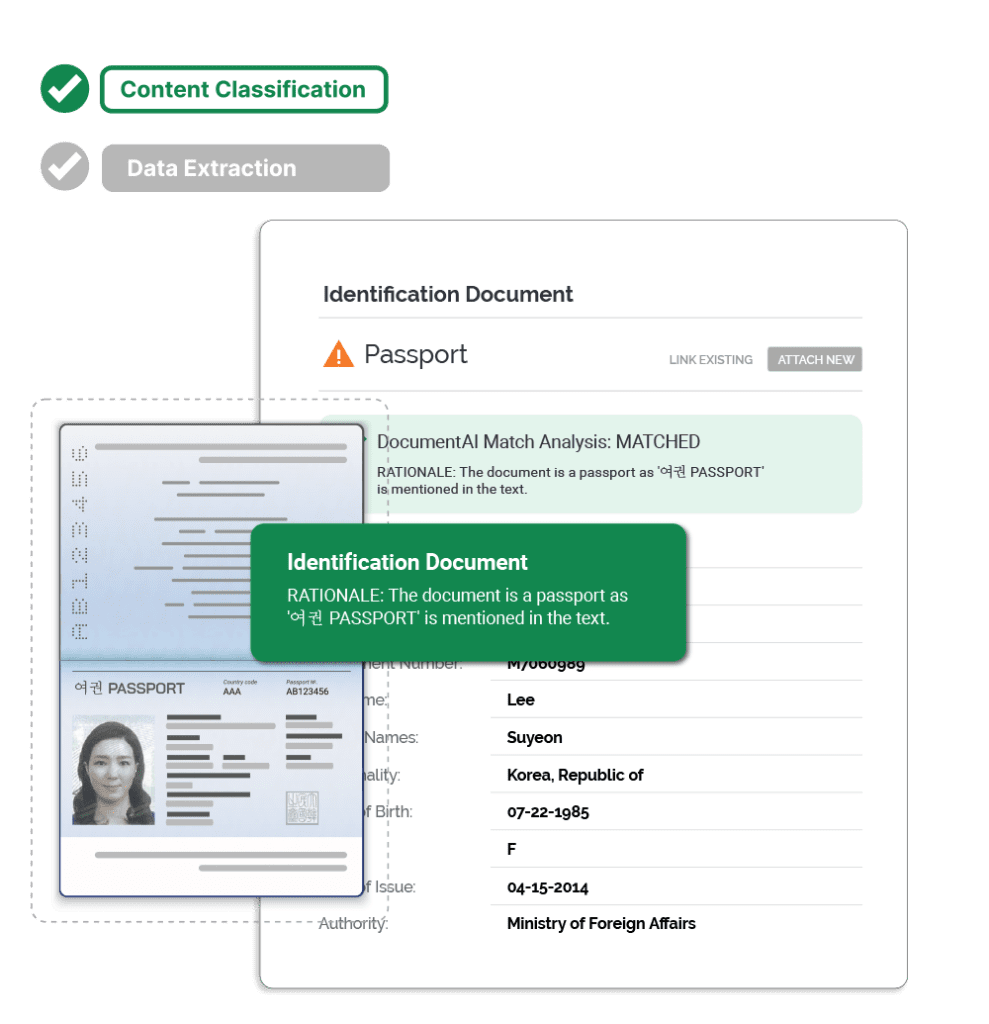
Using its Applied GenAI Process Automation framework, BizAI is able to apply the client’s reimbursement policies to all forms of billing templates to match and process the invoices while validating compliance standards — ensuring fast, accurate, and fully governed processing with zero data retention.
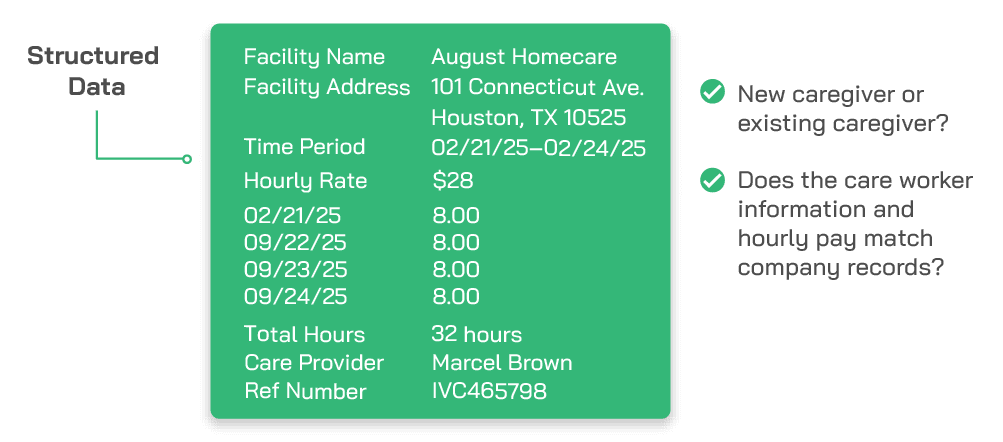
Structured outputs flow to AP, claims management, and compliance systems for payment decisioning.
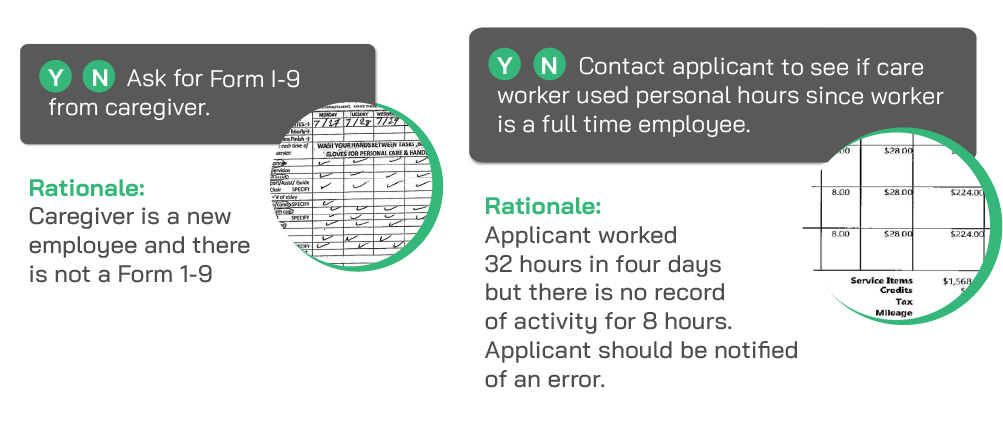
Non-compliant, duplicate, or unsupported invoices are routed directly to the compliance team with highlighted discrepancies.
BizAI is able to apply internal audit standards and payer compliance rules, ensuring policy and program adherence.
Every extracted field and compliance decision is fully traceable back to the source invoice and governing policy clause.