
Healthcare Insurance / Managed Care

National Health Insurer managing a network of 250K+ physicians, clinics, and facilities

Provider Contracting, Onboarding, and Compliance
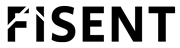
 The provider onboarding process in healthcare involves collecting and validating dozens of data points and compliance attestations before a provider can participate in the network.
The provider onboarding process in healthcare involves collecting and validating dozens of data points and compliance attestations before a provider can participate in the network.
Each new contract submission includes multiple unstructured artifacts — applications, W-9s, credentialing forms, service grids, and legal agreements — which vary across states, specialties, and product lines.
Contract administration teams were facing several challenges:
Using its Applied GenAI Process Automation framework, BizAI is able to apply the payer’s contract templates, state-specific policies, and internal workflows — ensuring a fully governed, audit-ready process without training on customer data or retaining any provider information.
BizAI outputs structured data to CRM, CLM, and credentialing platforms. By integrating with several systems of record, BizAI enables automated workflow triggers such as record creation, data population, and exception routing.

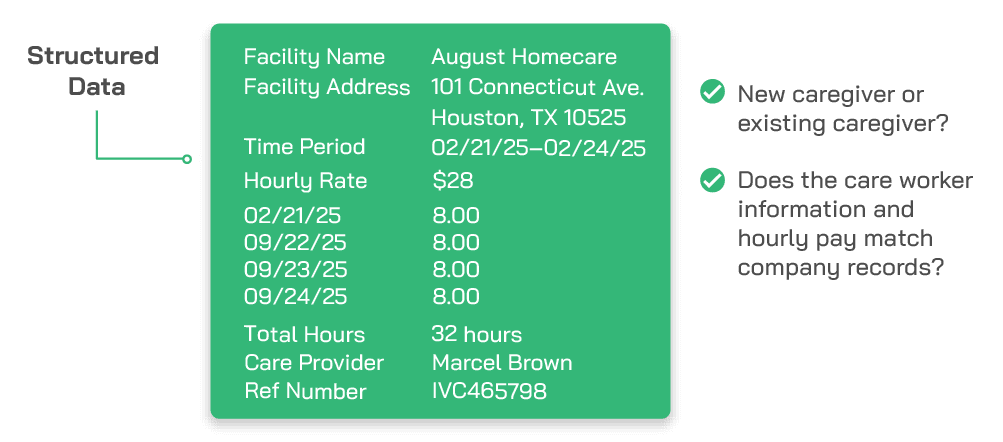
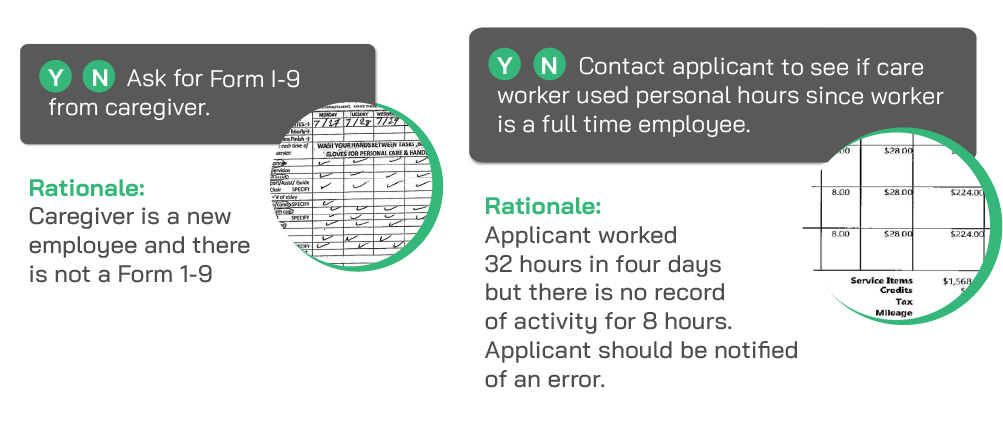
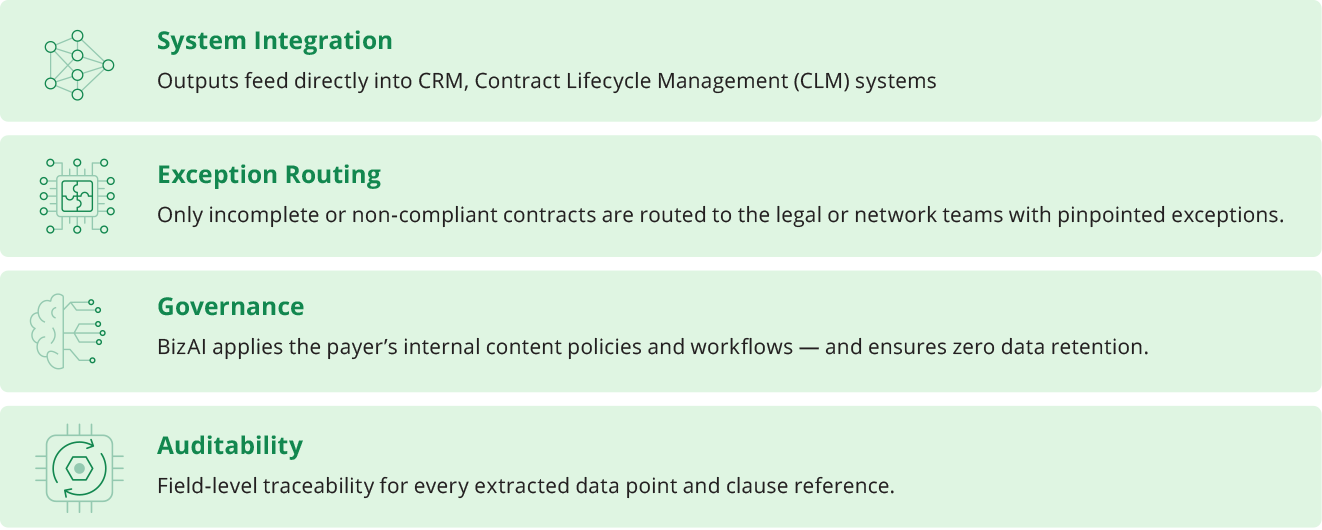
By digitizing and automating contract interpretation, BizAI establishes a single source of truth for provider contracts. It eliminates variations in how different teams interpret or key terms — creating a standardized, repeatable onboarding process that meets regulatory and operational compliance.
>90% faster onboarding for standard provider agreements.

95%+ data extraction accuracy across all contract types.
Reduction in compliance exceptions through consistent detection of state-specific clauses.
Improved transparency and audit readiness for CMS and state reviews.

Significant labor savings across legal, credentialing, and contracting teams.